The aim is to contribute to surgery and radiotherapy planning, by means of image registration, image segmentation and Monte Carlo simulations.
Image processing techniques have been proposed to facilitate pre-surgical planning, intra-surgical decision making and intra-operative radiotherapy dosimetry.
Intraoperative radiotherapy has the drawback that the computation of dosimetry cannot be done in advance, as the position of the tissues when applying the therapy cannot be accurately predicted.
To make feasible the therapy planning, we have worked in a fast method to compute radiation dose distribution with real images acquired during surgery. The method is based on a fast and customized Monte Carlo algorithm to compute dose distribution and has been integrated in radiance, GMV's treatment planning system.
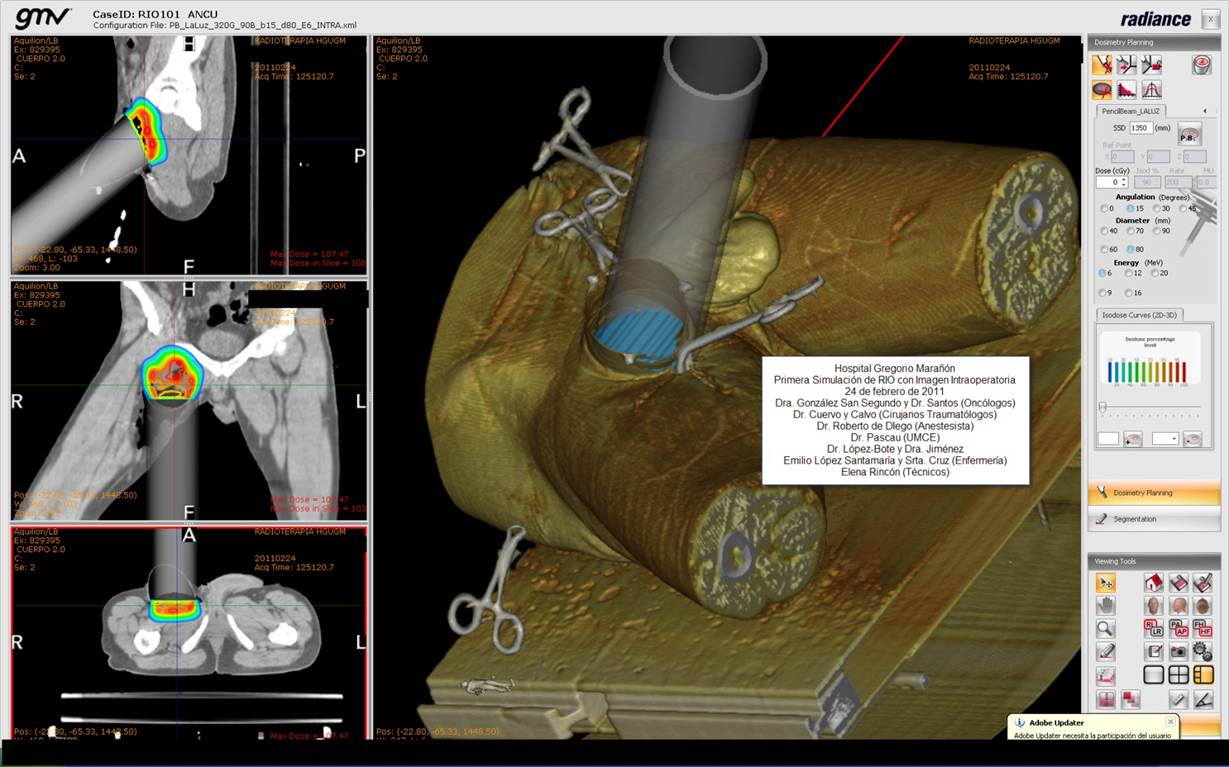
Treatment planning system showing the computed dose distribution in a clinical scenario
Essential parameters for liver surgery planning are the location of tumors, their position in relation to the vasculature and the volume of the remnant functional liver after the surgery. Automatic estimation of these parameters from preoperative CT or MRI studies aid surgeons to accurate plan hepatic surgery.
Image processing techniques (segmentation and registration) allows to obtain these parameters, combining information from both image modalities. In particular, we have proposed a new registration technique (organ-focused mutual information nonrigid multimodal registration) that is able to accurately combine liver anatomic CT with functional contrast-enhanced MRI.
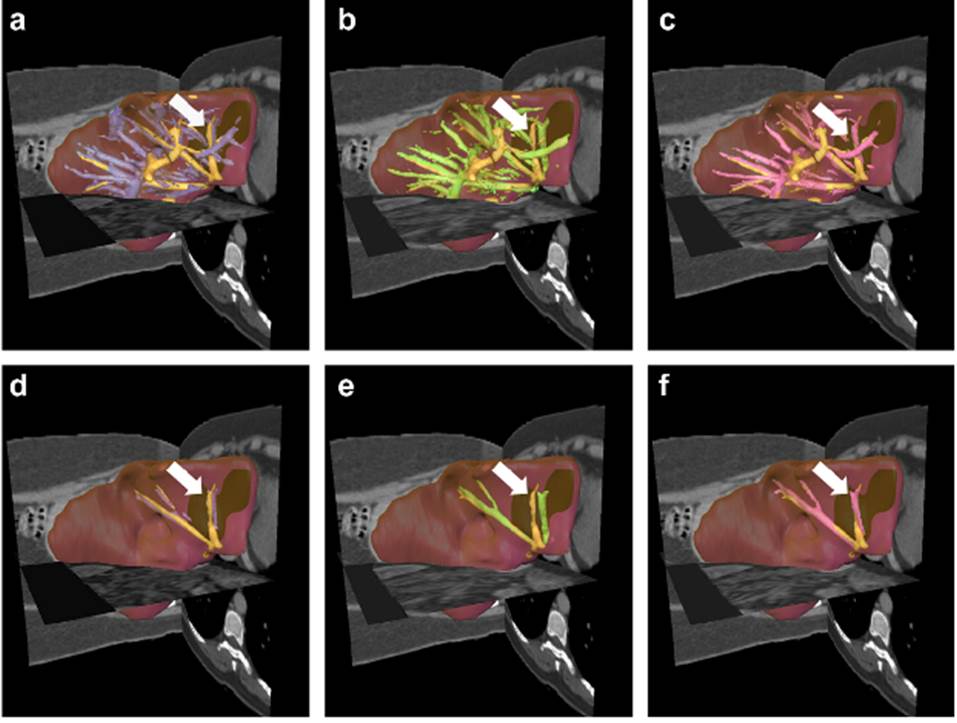
Organ-focused mutual information for nonrigid multimodal registration of liver CT and Gd–EOB–DTPA-enhanced MRI. Left-column: before registration, middle column: conventional MI registration; right column: MI registration with spatial information. Orange: vessels from CT; Purple, green, pink: vessels from MRI.
The accurate localization of the epileptogenic focus in epileptic patients that do not respond to drug medication, is critical to guarantee success in surgery treatment. One technique commonly used for this localization is the subtraction of Ictal SPECT Co-registered to MRI (SISCOM). SISCOM involves the registration of ictal and inter-ictal SPECT, intensity normalization, subtraction and registration of the result to an anatomic MRI image
In collaboration with Hospital Clínic, we have developed a tool (FocusDet) to aid clinicians in the analysis of these images and to locate the epileptic focus. Its accuracy has been evaluated with Monte Carlo simulations
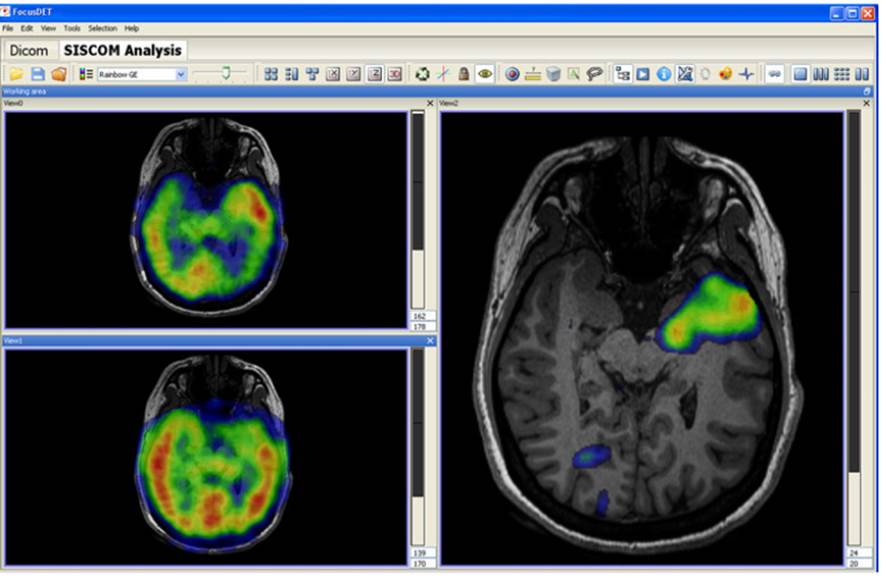
Ictal SPECT (top left), interictal SPECT (bottom left) and their subtraction (right) showing the localized epileptic focus. All the images are merged with the MRI (in gray).
This material is presented to ensure timely dissemination of scholarly and technical work. Copyright and all rights therein are retained by authors or by other copyright holders. All persons copying this information are expected to adhere to the terms and constraints invoked by each copyright holder. Permission to reprint/republish this material or to reuse any copyrighted component of this work in other works must be obtained from the copyright holders.
Copyright © 2005-2020 BIT-UPM. Map of web.
Last modified on 5 Aug. 2020 by andres@die.upm.es